Healthcare operations hinge on accuracy and speed. Patient intake, eligibility checks, and prior authorization often span EHR screens, payer portals, spreadsheets, and emails—creating delays, rework, and risk.
ZAPTEST streamlines this end‑to‑end workflow. By combining UI and API automation with AI + Computer Vision, teams standardize processes across systems, reduce manual rekeying, and produce audit‑ready evidence without adding IT burden.
The Problem
- Front‑desk teams collect demographics and insurance data, then retype it into the EHR.
- Staff verify eligibility on payer portals, capture screenshots, and update spreadsheets or the EHR.
- Clinicians request authorizations via web forms or uploaded PDFs; teams chase status by email.
- Documents (IDs, referrals, lab orders) live across inboxes and shared drives, complicating audits.
- Inconsistent steps cause delays, errors, and poor visibility into work queues.
How ZAPTEST Automates It
Capture and standardize the workflow
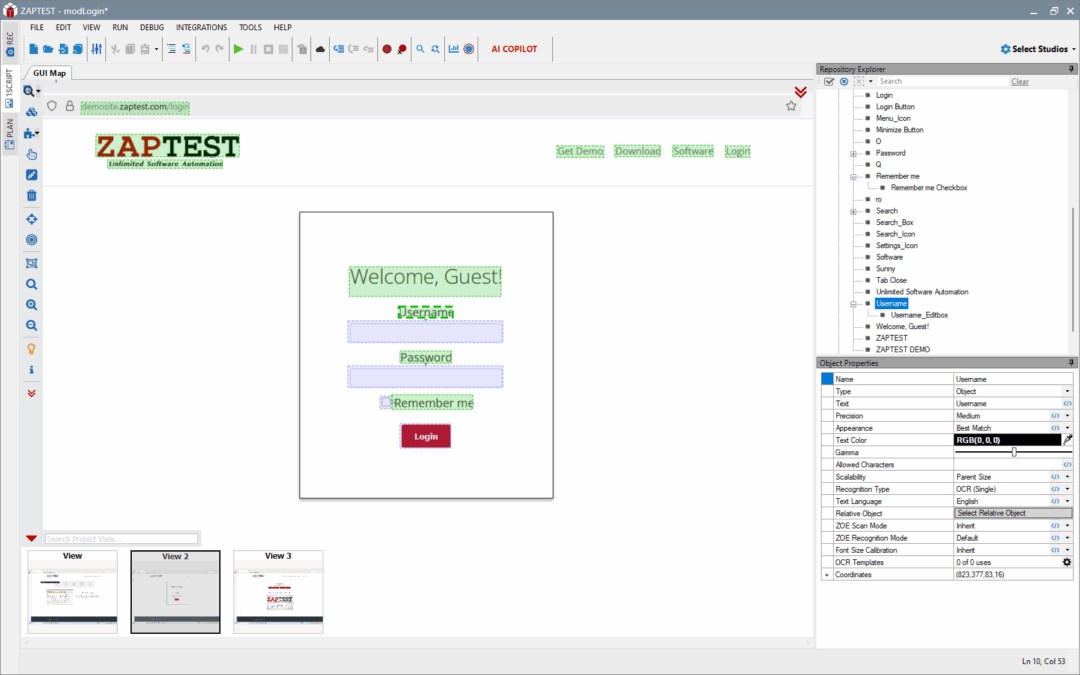
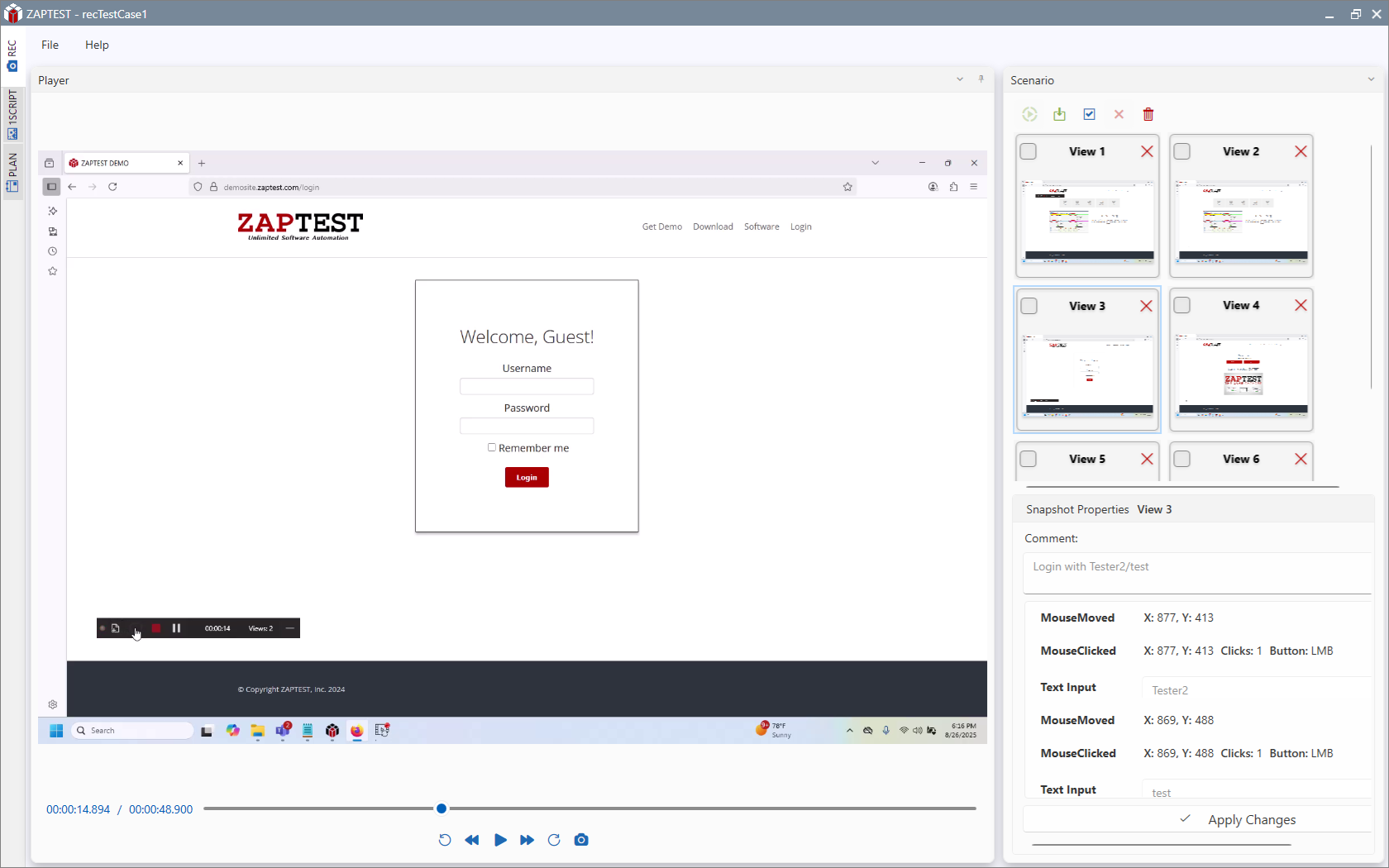
- REC Studio captures the current intake and authorization steps end‑to‑end across EHR, portals, and email.
- PLAN Studio converts tasks into reusable components (patient search, eligibility check, auth submission) for consistent execution.
Execute reliably across any UI
- ZOE (AI + Computer Vision) interacts with EHR screens and payer portals—even in virtualized or changing UIs—reducing brittle selectors.
- 1SCRIPT runs the same workflow across clinic locations, different browsers, and mixed environments without rewrites.
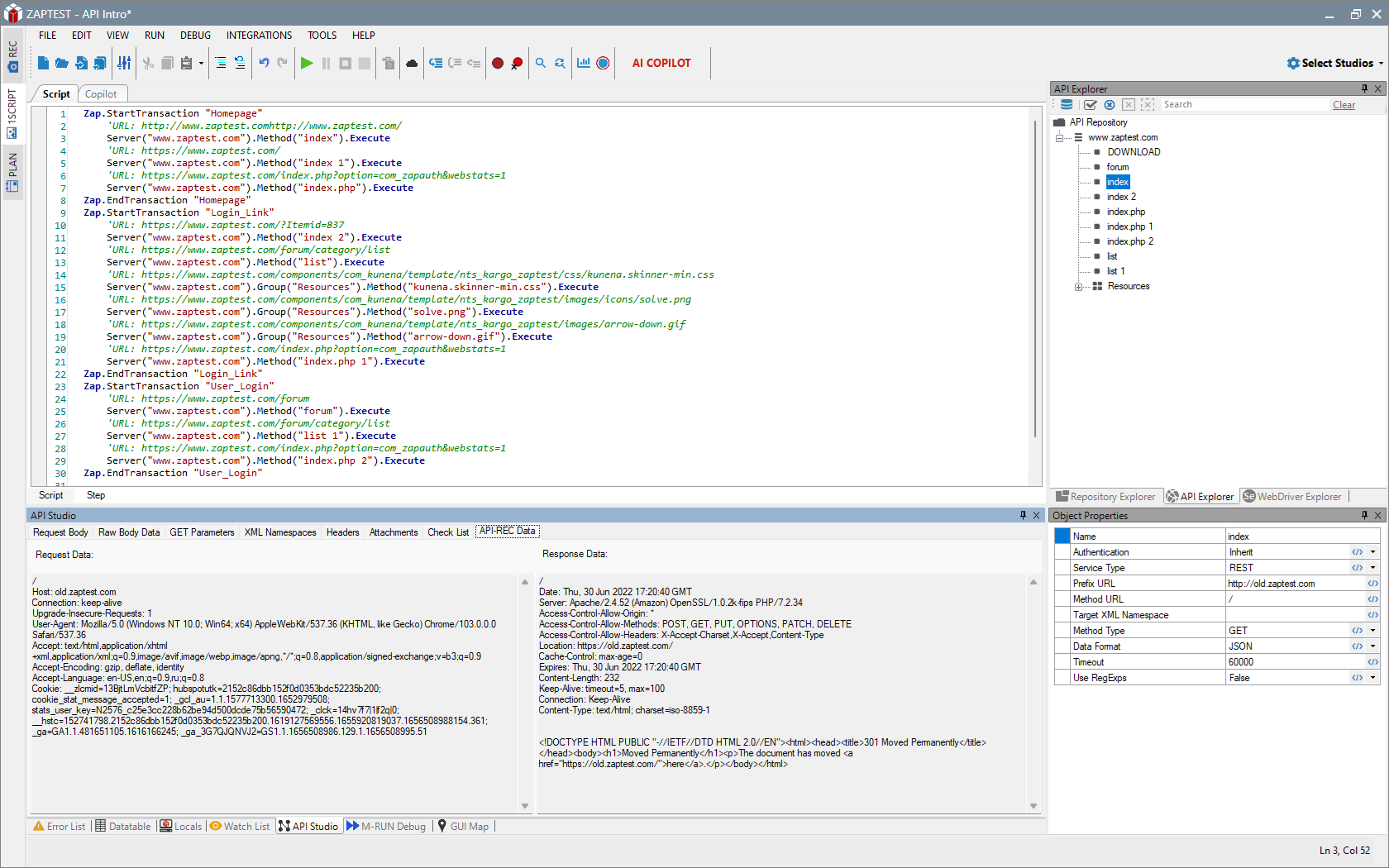
Use APIs where available; fall back to UI when not
- API Automation performs real‑time eligibility checks, pulls authorization status, and writes updates directly when endpoints exist.
- When APIs are unavailable, ZOE drives the portal UI to submit requests, upload documents, and capture confirmations.
Handle emails, documents, and data at scale
- Outlook Object Model monitors inboxes for payer responses, parses messages, and routes attachments.
- Word/Excel Object Models generate cover letters and maintain worklists without manual effort.
- Datatable Parameters run bulk validations for daily patient rosters and referral queues.
- FSO applies standardized naming (MRN/Date) and filing rules for IDs, referrals, and approvals.
- ADODB/DB ops reconcile EHR records with a data mart or reporting database for accuracy checks.
Visibility, evidence, and control
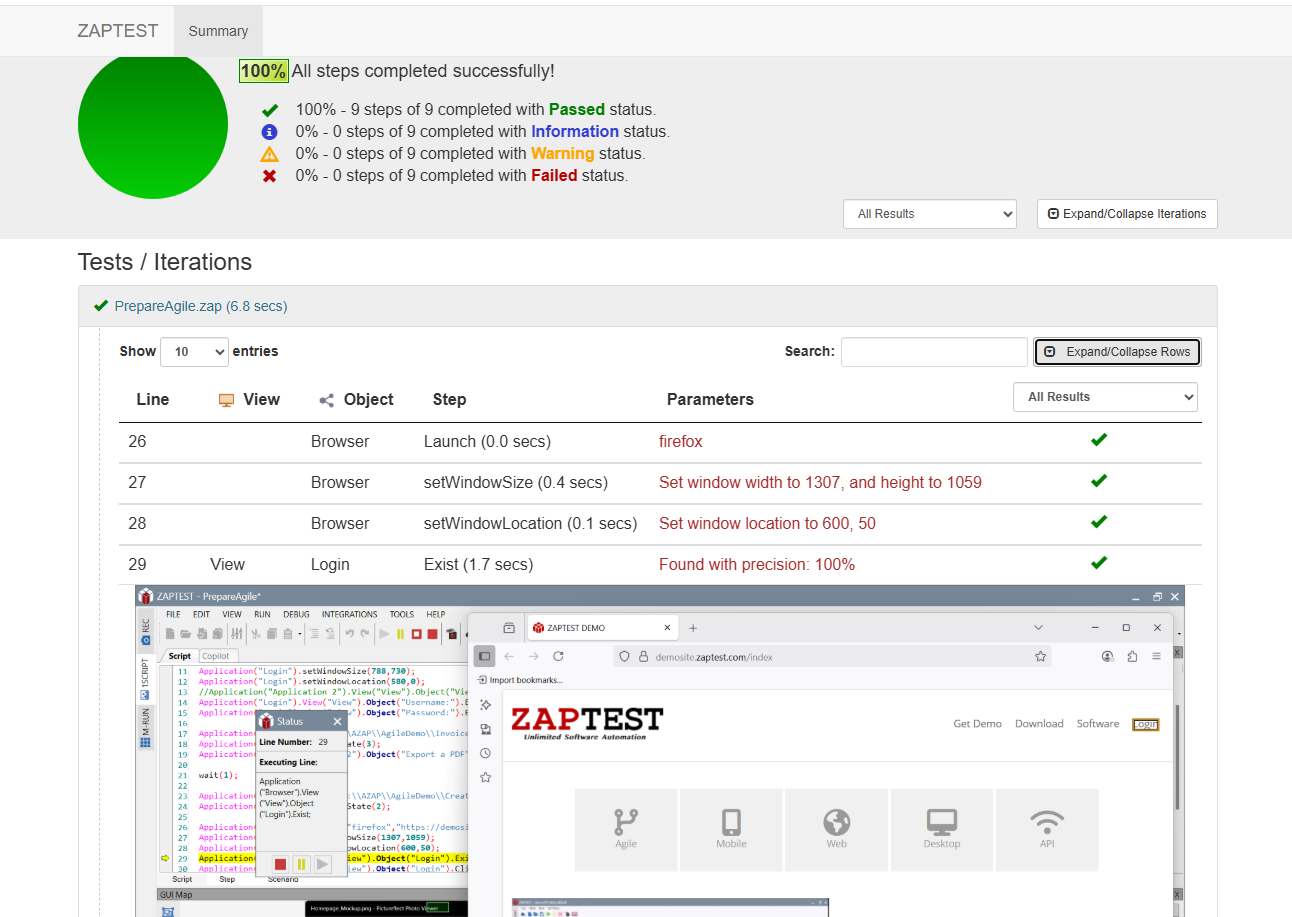
- Built‑in Reporting stores logs, screenshots, and outcomes for audit trails and QA review.
- Task Scheduler/CLI runs unattended batches (e.g., nightly eligibility pre‑checks) and dispatches alerts on exceptions.
Results
- Fewer manual re‑entries and copy‑paste errors across EHR and payer portals.
- Shorter authorization lead times through parallelized checks and automated submissions.
- Higher first‑pass accuracy with standardized, component‑based steps.
- Centralized, audit‑ready evidence for operational oversight.
- Scalable automation that adapts to UI changes and new payer requirements.
Conclusion
ZAPTEST unifies intake, eligibility, and prior authorization into a single, resilient automation fabric—combining UI automation, APIs, document handling, and audit reporting. Ready to accelerate care and reduce operational friction? Book a demo with ZAPTEST to see it on your data and systems.